24 Jul “Don’t give up just because your Medi-Cal renewal is late”
Even if you miss the submission date, there is an opportunity up to 90 days
Submit renewal form and report changes
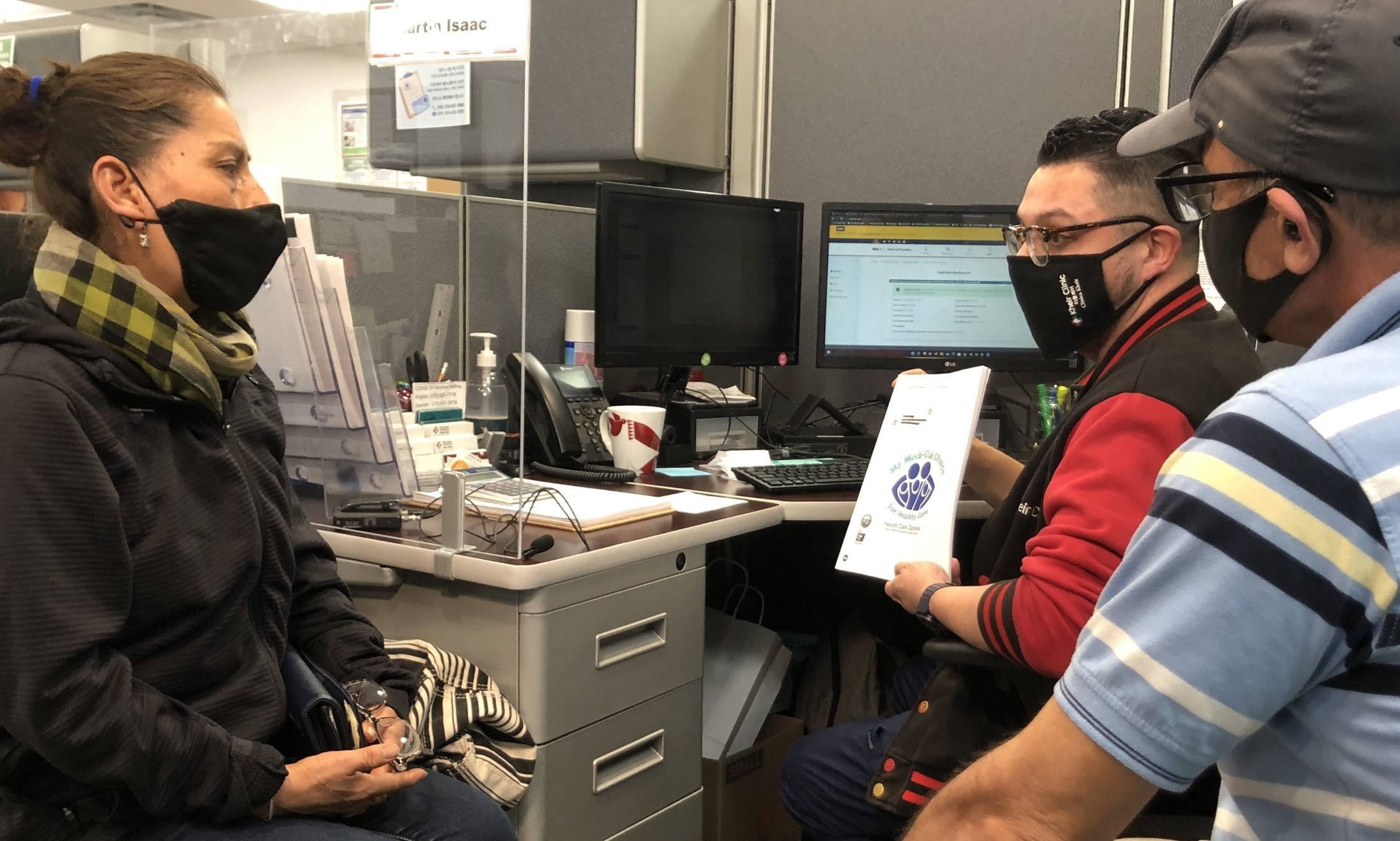
As the Public Health Emergency (PHE) ended in May, Medi-Cal redetermination was resumed and processing began in April for renewal due in June. As a result, number of recipients who lose their benefits increased. Kheir Clinic (CEO Erin Pak) encourages people not to give up even if you missed the renewal date, saying that there is still a chance to renew.
So far, the first redetermination process began in April for recipients whose need to renew their Medi-Cal in June. Those recipients, lose their coverage from July 1st if renewal documents are not submitted or if they are no longer eligible for Medi-Cal. Annual renewal is, typically, due in the 11th month after the application month, and same month every year thereafter. For example, if you applied in July 2022, your annual renewal due month is June.
Renewal form is sent to the beneficiary via mail in 60 days prior to Medi-Cal renewal end date, and you must submit or provide the requested information to DPSS within 60 days of receiving the documents, or by the due date indicated on the letter in the package, to prevent any lapse in coverage. If DPSS does not receive the renewal form or the information needed to redetermine continued eligibility, your eligibility worker from the county where you live contact you by phone or in writing after 30 days since the annual renewal form was sent, and remind you to submit.
Medi-Cal does not stop immediately if the renewal due date has passed. If DPSS does not receive the form or the information by the annual renewal form due date, then DPSS will send a 10-day Notice of Action letter explaining the reason for discontinuance from Medi-Cal and give warning “If you do not take action to renew within 10 days, you will lose your coverage.” If you miss your renewal form due date but receive this letter, submit the information or documentation before the Medi-Cal renewal end date and DPSS will rescind the discontinuance and complete the eligibility redetermination to avoid a lapse in coverage and send the approval Notice of Action letter.
Joanna Shin, a Health Education, Enrollment, and Outreach Specialist at Kheir, said, “The number of people in panic or discouragement who call or visit and ask what to do after they lose Medi-Cal benefits has increased significantly this month.” She added, “Please do not give up, submit information and documents, and check with your eligibility worker at DPSS.”
Because a beneficiary that is discontinued from Medi-Cal for failing to provide needed information or documentation is entitled to a 90-Day Grace or Cure Period. A 90-Day Grace / Cure Period reinstates discontinued Medi-Cal benefits when you submit information or documents requested and are found eligible. Then, the discontinuance will be rescinded and the beneficiary’s eligibility will be retroactively restored back to the discontinuance date.
Shin warned, “But after these 90 days, you have to apply for Medi-Cal all over again,” and added, “The renewal review is not over on June 30th. This was the first period after resumption of redetermination and it will be annually.” “If there is a change in personal information including address, phone number, email address over the past 3 years, be sure to report the county where you live now of these changes.” he emphasized.
Submit renewal documentation or needed information and report changes can be done by mail (to the address shown in the renewal package), online (www.BenefitsCal.com, www.CoveredCA.com), by phone (866-613-3777) or in person by contacting your county Department of Public Social Services (DPSS).
▶Inquiry: (213)632-5521 text, INFO@LAKHEIR.ORG email

